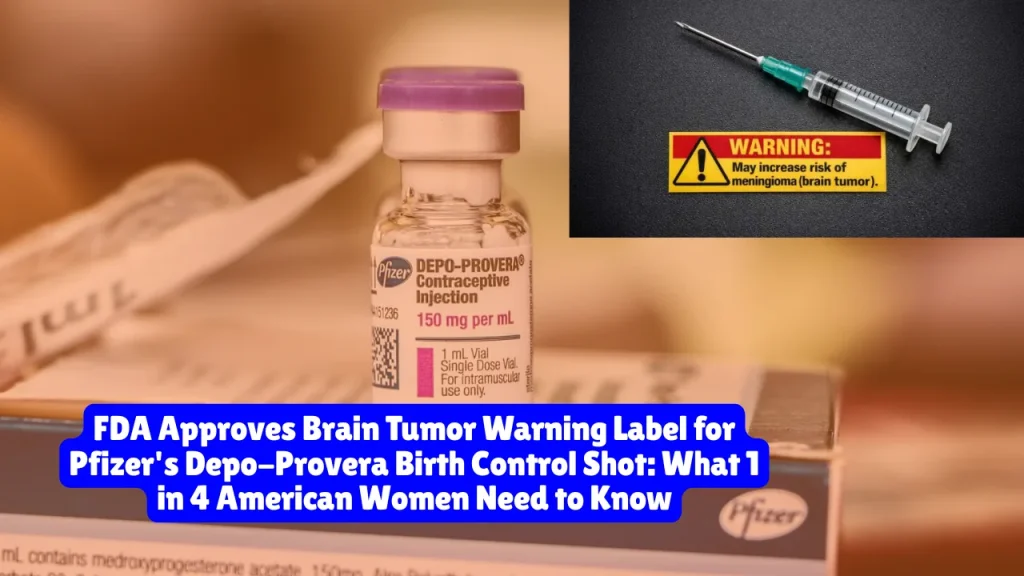
FDA Approves Brain Tumor Warning Label for Pfizer’s Depo-Provera Birth Control Shot, What 1 in 4 American Women Need to Know
The FDA approved a label change on December 13, 2025 requiring Pfizer to warn patients about meningioma, a tumor in the lining of the brain, for its Depo-Provera birth control shot. More than 1,000 women are suing Pfizer, claiming the company knew about brain tumor risks for decades but failed to warn American patients. Women who used Depo-Provera for over one year face a 5.5-fold increased risk of developing meningioma compared to non-users.
What the FDA Warning Says
The FDA approved warnings for two versions of the injection:
- Depo-Provera CI
- Depo-Subq Provera 104
The newly approved label states: “Meningioma cases have been reported with repeated use. Physicians should inform patients with a history of meningioma about the potential risk.”
Why This Matters Now
According to the Centers for Disease Control and Prevention, 1 in 4 sexually active women in the United States have used Depo-Provera. That’s millions of American women potentially at risk.
The FDA previously rejected a similar warning in 2024, making this approval a major reversal. Canada and Europe have warned about meningioma risks since 2022-2024, but American women received no such warning until now.
What Is Meningioma?
Meningiomas are tumors that form in the protective layers surrounding your brain and spinal cord. Most are non-cancerous, but they can still cause serious health problems depending on their size and location.
Approximately 39,000 meningiomas are diagnosed annually in the U.S.
Your Risk Level
Women using Depo-Provera may be up to 5.5 times more likely to develop meningioma compared to non-users.
Critical findings from research:
- No increased risk for women who used Depo-Provera for less than 1 year
- Risk begins rising after 1 year of use (4 injections)
- Highest risk for women who used it 5+ years
- About 75% of affected women used Depo-Provera for over 3 years
- Two-thirds of diagnosed women were over age 45
A February 2025 University of British Columbia study found approximately 1 in every 1,111 women receiving quarterly injections for a year may develop a brain tumor.
Related article: Frigidaire Ovens Exploding at Night While Owners Sleep, 900+ Complaints, Glass Shooting Across Kitchens

Symptoms Every Depo-Provera User Should Watch For
Meningiomas grow slowly, so symptoms may not appear for years. Watch for:
Most Common Warning Signs:
- Persistent headaches (77% of patients report this)
- Vision problems or blurry vision
- Cognitive issues or memory problems
- Hearing loss or ringing in ears
- Seizures
- Weakness in arms or legs
- Balance problems
- Confusion or personality changes
Less Common But Serious:
- Unexplained weight changes
- Loss of smell
- Numbness or tingling
- Speech difficulties
- Nausea or vomiting
If you’ve used Depo-Provera for over a year and experience any of these symptoms, contact your doctor immediately and request brain imaging.
What Current Users Should Do Right Now
1. Don’t panic, but don’t ignore this
Most women who use Depo-Provera will not develop meningiomas, but the risk is real.
2. Talk to your healthcare provider immediately
Discuss whether you should continue using Depo-Provera or switch to alternative birth control.
3. Consider your usage history
Have you used it for less than a year? Your risk is minimal. More than a year? Discuss screening options with your doctor.
4. Know your alternatives
Other birth control options include IUDs, oral contraceptives, patches, rings, and implants. Your doctor can help you choose what’s right for you.
5. Don’t stop suddenly without a backup plan
If you decide to discontinue Depo-Provera, have alternative contraception ready to prevent unintended pregnancy.
What Former Users Need to Know
If you stopped using Depo-Provera years ago, you still face elevated risk. Meningiomas can develop years after you stop the injections.
You should:
- Monitor yourself for symptoms listed above
- Tell your doctor about your Depo-Provera history
- Request screening if you experience persistent headaches, vision changes, or neurological symptoms
- Keep records of how long you used it and when
Former long-term users (5+ years) face the highest risk and may benefit from baseline brain imaging even without symptoms.
The Scientific Evidence Behind the Warning
March 2024 British Medical Journal Study:
Researchers analyzed over 108,000 women in France and found those who used Depo-Provera faced 5.55 times higher risk of meningiomas compared to non-users.
July 2025 Study:
Compared safety of medroxyprogesterone acetate to other oral contraceptives. Women using it for over a year were 3.5 times more likely to develop meningiomas.
Studies dating back to 1983:
Research showed links between progesterone and meningioma growth. Plaintiffs argue Pfizer should have investigated sooner.
Meningiomas often have receptors that respond to progesterone. Depo-Provera contains medroxyprogesterone acetate, a synthetic progesterone, which may encourage tumor growth.
Over 2,000 Women Are Suing Pfizer
As of December 2025, more than 2,000 women across the United States have filed lawsuits against Pfizer alleging:
- The company knew about brain tumor risks for decades
- Pfizer failed to warn American patients despite warning those in Canada and Europe
- The company had an “unassignable duty to investigate” based on 1983 studies
- Pfizer deliberately submitted inadequate warning proposals to the FDA knowing they’d be rejected
The cases are consolidated in a federal multidistrict litigation (MDL) in the Northern District of Florida before Judge M. Casey Rodgers.
Current litigation status:
- Nearly 1,500 cases in federal MDL as of December 2025
- Hundreds more in various state courts
- Roughly 9,500 additional claims under investigation
- First bellwether trials expected late 2026 or early 2027
Why American Women Weren’t Warned Sooner
Timeline of Pfizer’s actions:
- 1983-2023: Studies showed progesterone-meningioma link, but Pfizer took no action
- 2023: Pfizer claims it first became aware of meningioma risks
- February 2024: Pfizer submitted label change to FDA
- 2024: FDA rejected the initial request, saying evidence didn’t support warning for all MPA products
- June 2025: Pfizer resubmitted amended application
- December 13, 2025: FDA approved the warning
The controversy:
Plaintiffs’ attorneys argue Pfizer intentionally submitted a “half-baked request” to the FDA in 2024, knowing it would be rejected, so they could use the rejection as a legal defense claiming federal preemption.
Attorney Ellen Relkin stated: “It’s the new tool book. Give a half-hearted, half-baked request to the FDA, hoping that it’s denied because of its inadequacy, and then once they got the rejection, that’s their litigation defense.”
Court transcripts show large sections redacted, including passages about what safety information Pfizer provided to European regulators versus U.S. regulators.
International Warnings Pfizer Added Years Ago
Canada: Meningioma warning added to Depo-Provera labels as early as 2022
European Union: The European Medicines Agency added meningioma as a “possible side effect” in 2024
United Kingdom: Pfizer’s UK label already included brain tumor warnings
Yet American women received no such warnings until December 2025.
What Pfizer Says
Pfizer maintains: “Pfizer stands behind the safety and efficacy of Depo-Provera, which has been used by millions of women worldwide and remains an important treatment option for women seeking to manage their reproductive health.”
The company:
- Has not admitted wrongdoing
- Claims lawsuits are without merit
- Says it will “vigorously defend itself”
- Declined interviews about the ongoing litigation
Pfizer argues the FDA’s 2024 rejection of the label change carried “the force of law” and shields them from liability.
What Plaintiffs’ Attorneys Say
Lawyers representing affected women issued this statement:
“For years, Pfizer misled doctors, patients, and the FDA about Depo-Provera’s link to meningiomas, resulting in the needless suffering of thousands of women who developed these dangerous brain tumors. Pfizer’s knowledge of this risk goes back decades, yet there was no warning provided. We applaud the FDA in finally requiring this label change to better inform and protect women.”
Why Black Women Face Disproportionate Risk
Black women use Depo-Provera at nearly twice the national average, raising concerns about disproportionate health impacts.
Research shows:
- Black women were historically targeted for Depo-Provera promotion
- Lower-income women use it more frequently due to affordability and convenience
- Healthcare inequities mean these women often receive less counseling about risks
- Many learned about meningioma risks only after diagnosis
This creates a racial and economic justice issue, with marginalized communities bearing greater risk from inadequate warnings.
How This Affects Pfizer’s Legal Defense
The FDA’s approval of the warning label significantly weakens Pfizer’s federal preemption defense.
Before: Pfizer argued the FDA’s 2024 rejection meant they couldn’t add warnings, preempting state failure-to-warn lawsuits.
Now: The FDA approved warnings, undermining claims they were prevented from warning consumers.
Legal experts note manufacturers can update warnings independently using the “Changes Being Effected” (CBE) pathway without advance FDA approval when safety concerns arise.
Judge Rodgers previously stated she wouldn’t rule on Pfizer’s motion to dismiss until after the FDA made its labeling decision. That ruling is expected mid-2026.
Medical Monitoring Class Actions
Beyond individual injury lawsuits, class actions seek medical monitoring for millions of Depo-Provera users who haven’t been diagnosed with meningiomas yet.
These lawsuits argue Pfizer should pay for:
- Regular brain imaging for long-term users
- Neurological examinations
- Ongoing monitoring for early tumor detection
Plaintiffs claim they’re entitled to this monitoring given Pfizer’s failure to warn allowed continued exposure without informed consent.
What Healthcare Providers Must Tell Patients
With the new FDA warning, healthcare providers are now required to:
- Inform patients about the potential link between Depo-Provera and meningiomas
- Discuss risks with anyone considering Depo-Provera
- Specifically warn patients with prior meningioma history
- Provide adequate information for informed consent
- Document these discussions in medical records
Failure to provide these warnings could expose providers to medical malpractice claims.
Alternative Birth Control Options
If you’re considering stopping Depo-Provera, discuss these alternatives with your doctor:
Hormonal Options:
- Birth control pills (lower hormone doses than Depo)
- IUDs (hormonal or copper)
- Implant (Nexplanon)
- Patch
- Vaginal ring
Non-Hormonal Options:
- Copper IUD (no hormones)
- Barrier methods (condoms, diaphragm)
- Fertility awareness methods
- Permanent sterilization
Each has different benefits, risks, and effectiveness rates. Your doctor can help you choose the best option for your health situation.
Do You Have a Legal Claim?
You may qualify to file a lawsuit if you:
- Used Depo-Provera for at least 1 year (4 injections)
- Were diagnosed with an intracranial meningioma
- Required surgery, radiation, or ongoing monitoring for the tumor
- Experienced health complications from the meningioma
Potential compensation includes:
- Medical expenses (past and future)
- Lost wages
- Loss of earning capacity
- Pain and suffering
- Emotional distress
- Loss of quality of life
- Punitive damages
Statute of Limitations
Every state has deadlines for filing lawsuits. These vary but typically range from 1-6 years from:
- The date you were diagnosed
- The date you discovered (or should have discovered) your injury was linked to Depo-Provera
Because the connection only became widely known in 2024, many women may still fall within their state’s filing deadline.
Don’t wait. Consult with a product liability attorney soon to preserve your rights.
What Evidence You Need
If you’re considering a lawsuit, gather:
Medical Records:
- Proof of Depo-Provera injections (dates, frequency, duration)
- Meningioma diagnosis records
- Brain imaging results (MRI, CT scans)
- Surgical reports
- Treatment records
- Ongoing monitoring documentation
Other Documentation:
- Prescription records
- Pharmacy records
- Healthcare provider notes
- Insurance records
- Employment records showing lost wages
Questions to Ask Your Doctor
If you’re currently using Depo-Provera:
- Should I continue using it given my health history?
- What are my alternative birth control options?
- Do I need baseline brain imaging?
- What symptoms should I watch for?
- How often should I be monitored?
If you’re a former user:
- Am I at increased risk given how long I used it?
- Should I get screened even without symptoms?
- What type of imaging do you recommend?
- How often should I be monitored?
- What symptoms warrant immediate evaluation?
The Broader Impact
This case highlights ongoing issues in pharmaceutical safety:
- Drug companies providing stronger warnings internationally than in the U.S.
- Delays in FDA action despite mounting evidence
- Federal preemption used as a litigation defense
- Racial and economic health disparities
- The need for stronger post-market surveillance
Advocates argue this case should prompt:
- Stricter requirements for updating safety warnings
- Greater transparency about international labeling differences
- Enhanced oversight of pharmaceutical companies
- Better informed consent processes
What Happens Next in Litigation
Short term (next 6 months):
- Judge Rodgers rules on Pfizer’s motion to dismiss
- More women file lawsuits as awareness spreads
- Discovery continues
- Parties prepare bellwether cases for trial
Medium term (late 2026-early 2027):
- First bellwether trials go to juries
- Outcomes influence settlement negotiations
- Additional scientific evidence may emerge
- Regulatory investigations may expand
Long term (2027+):
- Potential global settlement if bellwether trials favor plaintiffs
- Individual trials for cases not included in settlement
- Appeals of unfavorable rulings
- Implementation of any court-ordered safety measures
Frequently Asked Questions
I used Depo-Provera for 6 months. Am I at risk?
Research shows no increased risk for women who used it less than a year. However, tell your doctor about any neurological symptoms.
Can I get screened even if I have no symptoms?
Yes. If you used Depo-Provera for multiple years, talk to your doctor about baseline brain imaging.
Will my insurance cover screening?
Coverage varies. The new FDA warning may make it easier to get insurance approval for monitoring.
Are all meningiomas caused by Depo-Provera?
No. Meningiomas have multiple causes. However, long-term Depo use significantly increases risk.
What if I can’t afford a lawyer?
Most product liability attorneys work on contingency, meaning they only get paid if you win. Initial consultations are typically free.
How long do meningioma lawsuits take?
Product liability cases typically take 2-5 years. The MDL process may speed up or slow down individual cases depending on bellwether trial outcomes.
Can I sue if I haven’t been diagnosed with a meningioma?
Individual injury claims require a diagnosis. However, you may qualify for medical monitoring class actions.
What if my meningioma was surgically removed years ago?
You may still have a claim. Consult an attorney about your state’s statute of limitations.
Is Depo-Provera being recalled?
No. It remains on the market with the new warning label.
Should I get genetic testing?
Discuss this with your doctor. Some genetic factors may influence meningioma risk.
Important Reminders
- The FDA warning validates serious health risks
- 1 in 4 American women have used this product
- Symptoms may not appear for years after stopping
- Black women and lower-income women face disproportionate risk
- You have legal rights if you developed a meningioma
- Statutes of limitations vary by state – don’t wait
- Most product liability lawyers offer free consultations
- Current users should discuss alternatives with their doctor immediately
- Former users should monitor for symptoms and inform healthcare providers of their history
This article provides general information about the FDA’s Depo-Provera brain tumor warning and related litigation. It is not medical or legal advice. For medical guidance, consult your healthcare provider. For legal counsel, contact a product liability attorney.
About the Author

Sarah Klein, JD, is a licensed attorney and legal content strategist with over 12 years of experience across civil, criminal, family, and regulatory law. At All About Lawyer, she covers a wide range of legal topics — from high-profile lawsuits and courtroom stories to state traffic laws and everyday legal questions — all with a focus on accuracy, clarity, and public understanding.
Her writing blends real legal insight with plain-English explanations, helping readers stay informed and legally aware.
Read more about Sarah